California Management Review
California Management Review is a premier professional management journal for practitioners published at UC Berkeley Haas School of Business.
by Suhani Gupta and Vijaya Sunder M
Image Credit | djvstock
As virtual consultations, AI-driven diagnostics, and wearable health devices gain traction, healthcare is increasingly connected.1 Yet, these advancements raise critical questions: Are digital tools truly enhancing patient care, or are they creating a new kind of divide? This article explores the dual impacts of digital healthcare innovations on patient-provider relationships, and how healthcare leaders can balance technology with human connection.
Björkdahl, J., Holgersson, M., & Teece, D. J. (2024). “Digital Platform Grafting: Strategies for Entering Established Ecosystems.” California Management Review, 66(3), 27-46.
Garbuio, M., & Lin, N. (2019). “Artificial intelligence as a growth engine for health care startups: Emerging business models.” California Management Review, 61(2), 59-83.
Sunder M, V., & Modukuri, S. (2024). “Essential Capabilities for Successful Digital Service Innovation at the Bottom of the Pyramid.” California Management Review, 66(3), 69-92.
Digital innovations are reshaping healthcare delivery by increasing efficiency, broadening access, and personalizing care.2 They have the potential to strengthen patient-provider connections, yet the technology-driven approach risks diminishing the human touch that is central to effective care. This shift raises concerns about whether a heavy reliance on digital tools might lead to interactions that feel more transactional than personal.
Dr. Michael Howell, Chief Clinical Officer at Google Health, expressed excitement over the rapid adoption of AI in healthcare, but also cautioned about its risks.3 This is but one example of the ongoing debate over whether digital innovations in healthcare are truly enhancing care or perhaps introducing new forms of distance between patients and providers. The key challenge for healthcare leaders will be to balance the integration of digital innovations while preserving the human connection, which would continue to remain central to trust and effective patient care.
To harness the full potential of digital innovations, healthcare systems can integrate these technologies into different process bundles throughout the patient journey. We define process bundling as the grouping of related tasks and procedures into unified and cohesive groups. In line with past research on bundles,4 key factors when aligning tasks into bundles include – a common objective; involves similar nature of healthcare providers; leverages same skills and capabilities; shares resources; and targets specific segment of patient beneficiaries. As one views the process together as bundles, it helps avoid redundancy, enhances coordination, and streamlines care pathways. Further, in combination with other digital technologies, such as telehealth and actual-time sharing of health data, wearables, and AI-led tools, process bundling can further amplify these benefits. A structured integration of technology across patient journey ensures that these solutions enhance patient experience and treatment outcomes rather than detract.5
For instance, processes like diagnostic tests, imaging, and medical assessments can be grouped under “Diagnosis” bundle, powered by digital solutions, such as AI-powered diagnostic tools, remote imaging analysis, symptom analysis and digital health records. These tools streamline resources, improve diagnostic accuracy, reduce wait times, and delivers more coordinated patient care.
The entire patient journey can be divided into five digital process bundles: ‘Awareness’, ‘Diagnosis’, ‘Treatment’, ‘Adherence’, and ‘Control or Remission’ (see Figure 1). When digital tools are embedded seamlessly across these bundles, healthcare becomes efficient, responsive, patient-centric and enhances overall care experience. However, if mismanaged, it risks over-reliance on technology, leading to diminished human connection between patients and providers.
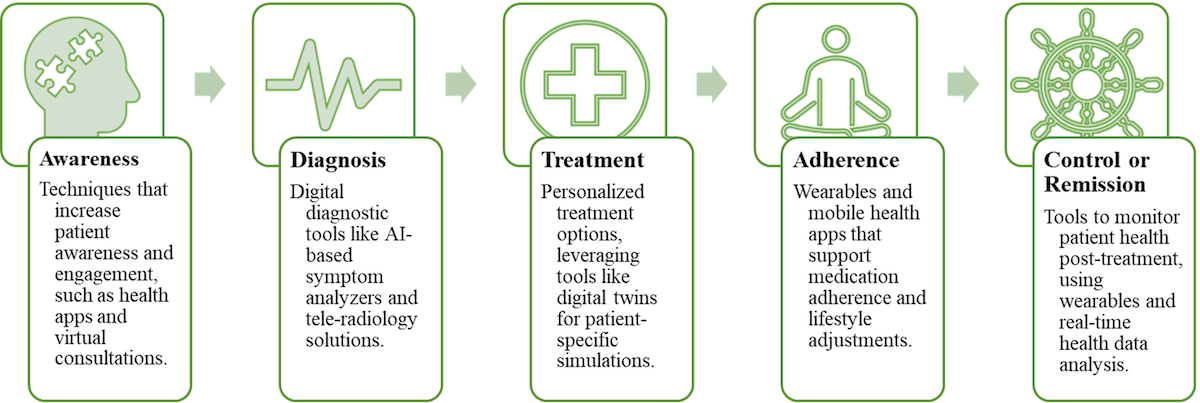
Figure 1. Process Bundles of Patient Journey for Digital Healthcare
Below, we illustrate three use cases across different phases of patient journey. Each example sheds light on how technology can enhance efficiency, personalization, and patient engagement, while also revealing potential risks such as reduced interaction, diminished trust, and over-reliance on technology. Analysing these use cases, we move closer to the core debate: Are digital innovations truly bridging the gap between patients and providers, fostering trust, or are they inadvertently creating distance by replacing critical human interactions with technology?
This is a technology application across process bundles ‘Awareness’ and ‘Diagnosis’.
In healthcare, patients often feel dissatisfied due to time constraints during consultation visits. A survey by Deloitte found that 63% of patients felt their questions were left unanswered during visits, highlighting the need for better communication approaches.6 This gap is bridged by emerging AI-powered symptom analysers that allow patients to input their symptoms in advance and generate reports for doctors to review prior to consultation. Ubie is one leading example of this innovation that enables patients to log their symptoms through an easy, user-friendly, quick questionnaire, creating summary diagnostic reports that patients can share with doctors prior to visit.
Reports generated by such AI-powered tools provide deeper understanding of the patient’s condition, reduce redundant questions, and helps providers to focus on critical issues during patient consultation. Therefore, through streamlined information flow, these tools enhance process efficiency and allow meaningful interactions in the limited consultation time, improving patient engagement.
However, these technologies also present challenges of undermining patient-provider trust. When much of the diagnostic process is pre-analysed by AI, doctors might engage with patients less directly, reducing opportunities for meaningful conversations that builds trust. Over-reliance on digital tools may lead to weaker human connections, making patients feel disengaged and sceptical about quality of care and reducing trust, and confidence on providers.7 Patients increasingly express their preference for involvement of a trusted human in cases of AI-driven healthcare decisions.8
The core challenge lies in balancing the efficiency of AI with the need for empathetic care. Healthcare providers must ensure that AI tools are used as supplements not as replacements to enhance patient engagements.9 By careful integration of AI into care journey, providers can not only improve diagnostic but also bridge communication gaps without compromising patient trust. The goal must be to leverage AI’s precision to promote strong patient-provider relationships, while ensuring technology complements rather than widens the divide in care delivery.
This is an advanced AI application across process bundles ‘Diagnosis’ and ‘Treatment’.
The advancement of digital twin technology in healthcare indicates a novel shift toward highly personalized medicines. Creating virtual patient care models can be personalised using patient data such as genetics, lifestyle, and health data.10 Digital twins enable healthcare providers to predict health issues, simulate treatment reactions, and build custom plans with accuracy. Platforms like Lami.fit leverage digital twin technology to offer proactive health management based on patient’s unique DNA and health profile, advancing care beyond what traditional methods can achieve.11
This level of personalization reduces the need for a broad, trial-and-error treatment approaches. Through data-driven insights, doctors can provide accurate diagnoses and targeted treatment plans, giving patients a sense of satisfaction that their care journey is uniquely tailored to their needs.
However, while digital twins offer unparalleled opportunities, they also introduce challenges that could displace experienced judgment of healthcare providers. As reliance on such data models grows, there is a risk that clinical expertise and intuition developed over years of practice could be overshadowed by algorithmic recommendations.12 Providers may begin seeing patients’ health as data in models, reducing their nuanced judgment of individual patient needs. Patients do not desire to be treated as data points in algorithms. They expect doctors to apply their clinical experience to interpret symptoms, balancing emotional and contextual factors that algorithms cannot capture. Algorithms can emulate human-like reasoning and behaviour, but they can never fully replicate the complexity of human intuition, empathy, and judgment. Further, use of extensive healthcare data may trigger privacy concerns among patients about how their personal health data is stored, shared, and used in modelling. If not handled with transparency and patient consent, it could diminish patient trust toward both technologies and healthcare providers using them.
This use case reflects the need to balance benefits of technology without displacing human judgment. Healthcare providers must ensure that digital twins serve as support tools, enhancing care by informing decisions, while leaving final judgment in the hands of experienced doctors. Preserving human connection and expert judgment is essential for sustaining relationships between patients and providers in a technology-driven healthcare landscape.
This is a device-driven technology across process bundles ‘Awareness’, ‘Diagnosis’, ‘Adherence’ and ‘Control’.
Wearable health monitoring devices, such as Apple Watch, Fitbit, and Oura Ring have increasingly become popular and widely adopted, offering patients real-time insights into their health, promoting proactive management of their fitness, sleep, and some chronic conditions. An advanced-level integration of these devices with electronic health records would enable healthcare providers to remotely monitor patient metrics, adjust treatment plans in real-time, and improve adherence to care. A study conducted by Evidation Health concluded that patients with chronic diseases who engage in activity tracking have significantly higher medication adherence than those who do not track their activities.13
However, wearables also introduce challenges that may strain doctor-patient relationships. Patients, equipped with self-tracked data, may feel empowered to make independent decisions regarding their health, sometimes even challenging professional recommendations.14 This can create friction between patients and providers and reduce the effectiveness of treatment outcomes. Additionally, patients may feel overwhelmed data overload and may overreact to allowable fluctuations as alarming signs. Without proper guidance on data interpretation, this can lead to unnecessary healthcare visits. Some patients also question the reliability and accuracy of their wearable devices, shifting discussion focus away from meaningful care towards addressing data discrepancies, consuming valuable doctor consultation time and reducing the quality of patient engagement.
To overcome these challenges, health providers must set realistic expectations to patients about the role of these wearable devices and actively guide patients on interpreting data. Wearables must be positioned as support technologies to enhance care and not replace professional care. When used effectively, these devices can enhance patient involvement for collaborative decision making and improve outcomes. However, this integration requires careful balance while preserving trust and meaningful interaction in the patient-provider relationship.
The above use cases reveal a recurring theme: while digital innovation in healthcare offer remarkable advancements in efficiency, personalization, and accessibility, it also presents challenges that can undermine trust and create a sense of detachment between patients and providers.
The following framework outlines the essential steps to integrate digital tools in a way that bridges the gap between technology and human connection, allowing healthcare providers to deliver care without compromising patient trust and human relationship at the core of healthcare. See Figure 2 for patient-centered digital integration framework, that we propose.
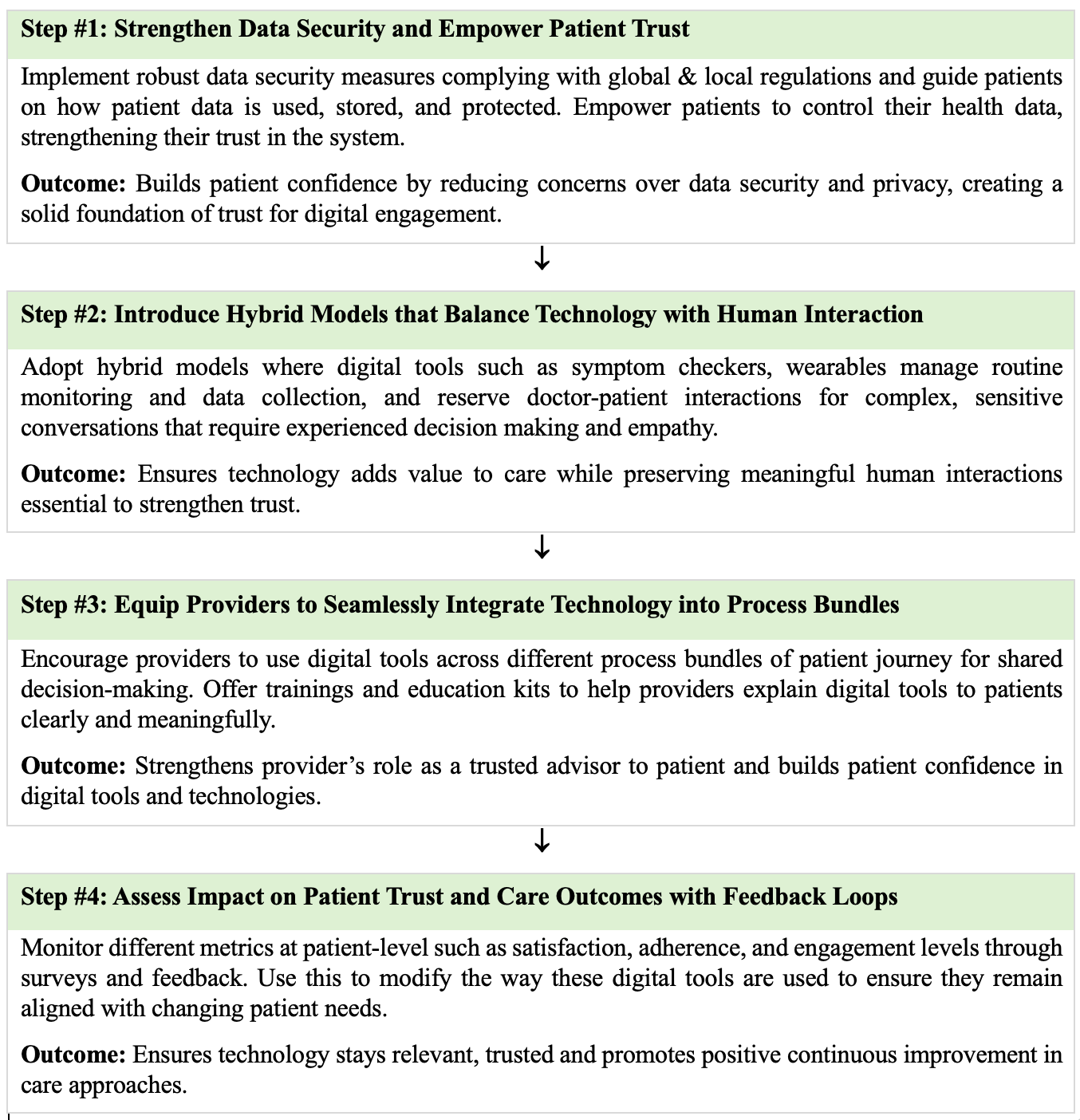
Figure 2. Patient-Centred Digital Integration Framework
In summary, we posit that while digital tools can make healthcare delivery more efficient, balancing these technologies with human interaction is essential. Healthcare leaders must not view digital integration as a choice between technology and empathy; instead, they should strive to integrate both elements to improve patient outcomes. Achieving this balance will lay the foundation for the next evolution in healthcare. Our framework provides healthcare leaders with a clear and actionable guide for integrating digital tools into healthcare process bundles while maintaining relationship and strengthening patient trust. The debate is not about choosing between technology or human interaction, but it’s about integrating both to improve patient experiences and outcomes - a balance that will form foundation of healthcare’s next evolution.
Björkdahl, J., Holgersson, M., & Teece, D. J. (2024). Digital Platform Grafting: Strategies for Entering Established Ecosystems. California Management Review, 66(3), 27-46.
Garbuio, M., & Lin, N. (2019). Artificial intelligence as a growth engine for health care startups: Emerging business models. California Management Review, 61(2), 59-83.
Parambath, A (2023). Medium, Retrieved from: https://medium.com/pear-healthcare-playbook/lessons-from-dr-33ad46383a09
Shah, R., & Ward, P. T. (2003). Lean manufacturing: context, practice bundles, and performance. Journal of operations management, 21(2), 129-149.
Sunder M, V., Modukuri, S., & Srivastava, R. K. (2022). A Value-Driven Digital Strategy Framework for Healthcare Firms. California Management Review. Retrieved from: https://cmr.berkeley.edu/2022/12/a-value-driven-digital-strategy-framework-for-healthcare-firms/
Reynolds, K. A. (2019). Patients don’t feel their doctors are compassionate, survey finds. Medical Economics. Retrieved from: https://www.medicaleconomics.com/view/patients-dont-feel-their-doctors-are-compassionate-survey-finds
Collina, L., Sayyadi, M., & Provitera, M. (2023). Critical Issues About AI Accountability Answered. California Management Review Insights. Retrieved from: https://cmr.berkeley.edu/2023/11/critical-issues-about-a-i-accountability-answered/
Longoni, C., Bonezzi, A., & Morewedge, C. K. (2019). Resistance to medical artificial intelligence. Journal of Consumer Research, 46(4), 629-650.
McGillin, F. (2024), Empowerment, Not Replacement: The Future of AI is Personal. Retrieved from: https://www.healthcareittoday.com/2024/10/02/empowerment-not-replacement-the-future-of-ai-is-personal/
Halamka, J. (2022), Can Digital Twins Improve Patient Care? Mayo Clinic, Retrieved from: https://www.mayoclinicplatform.org/2022/07/12/can-digital-twins-improve-patient-care/
Retrieved from: https://www.lami.co.in/
Łukaniszyn, M., Majka, Ł., Grochowicz, B., Mikołajewski, D., & Kawala-Sterniuk, A. (2024). Digital Twins Generated by Artificial Intelligence in Personalized Healthcare. Applied Sciences, 14(20), 9404.
Alvaro, D., Branch, E. (2020). Wearable Technology: Innovation, Adherence, and Clinical Outcomes. Pharma’s Almanac. Retrieved from: https://www.pharmasalmanac.com/articles/wearable-technology-innovation-adherence-and-clinical-outcomes
Hossain, M. (2022). Wearable Devices to Revolutionize Health Care. California Management Review Insights. Retrieved from: https://cmr.berkeley.edu/2022/08/wearable-devices-to-revolutionize-health-care